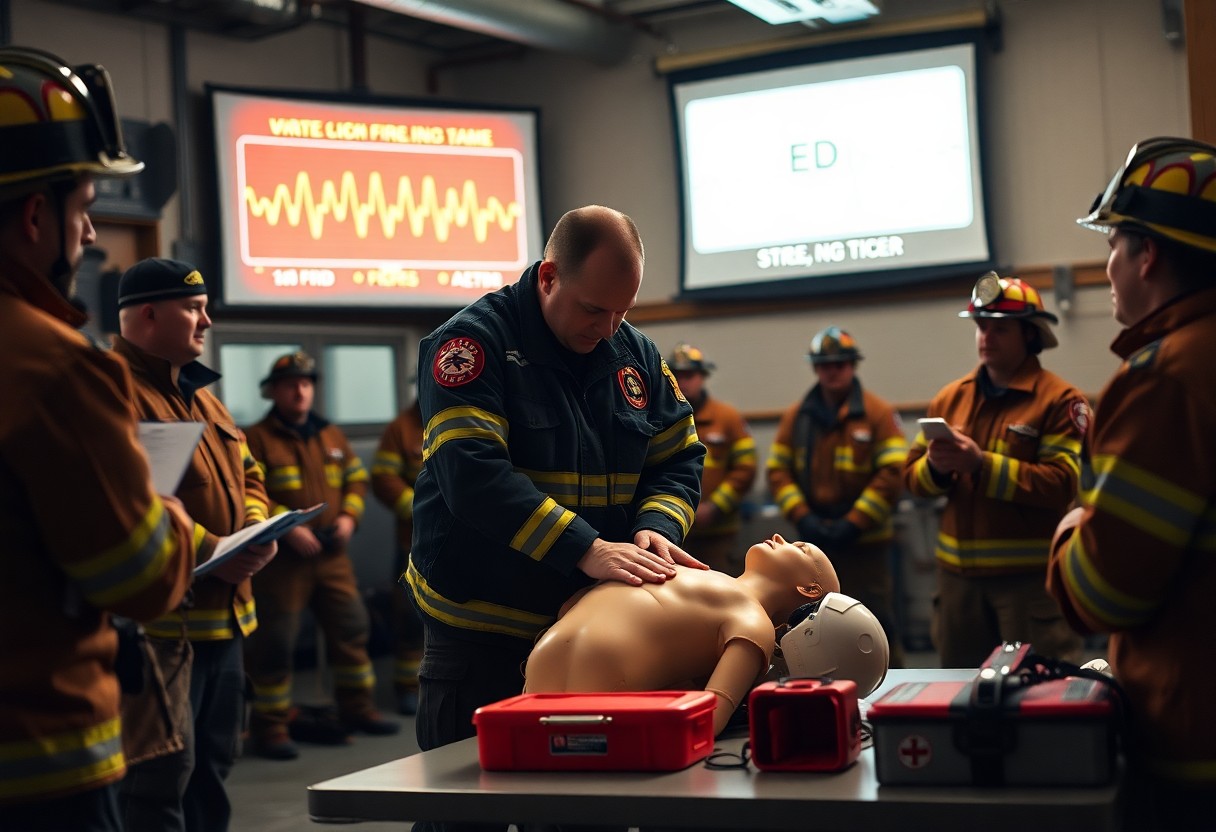
There’s a clear need for you as a volunteer fire chief to lead cardiac health initiatives by implementing regular screenings, CPR/AED training, fitness standards, and post-incident support to reduce on-duty cardiac events and protect team readiness.
Assessing the Cardiac Risk Profile in Volunteer Services
Assessing your service’s cardiac risk profile means combining incident data, member health screenings, and operational factors to target prevention, training, and AED placement based on measured need.
Statistical analysis of cardiovascular line-of-duty deaths
Analyzing your department’s line-of-duty cardiac events reveals patterns by age, activity, and response time to inform targeted screening and policy changes.
Identifying unique physiological stressors in volunteer environments
Recognizing your volunteers face unpredictable exertion, heat exposure, interrupted sleep and rapid call-response shifts lets you tailor fitness standards, hydration protocols, and rest policies.
Consider monitoring heart-rate trends, offering graded fitness tests, enforcing cooldowns after heavy exertion, and scheduling return-to-duty checks for older or high-risk members.
Implementing Mandatory Health and Wellness Screenings
You require routine cardiac screenings for all members and enforce follow-up for abnormal results, making assessments part of duty readiness.
Standardizing NFPA 1582 compliant physicals
Require NFPA 1582-compliant physicals annually, ensuring ECGs, lipid panels, and blood pressure checks are documented and tracked for every firefighter.
Establishing partnerships with local healthcare providers
Connect with nearby hospitals and clinics so you can arrange on-site screenings, expedited referrals, and educational sessions tailored to firefighters’ cardiac risks.
Work with hospital cardiology departments, occupational health clinics, and EMS medical directors to negotiate reduced-cost ECGs, stress tests, and cholesterol screenings for your crew. Set memoranda of understanding that define on-site clinic schedules, referral pathways, and confidential result reporting. Schedule quarterly educational briefs and joint drills so your team gains timely access to specialist care and clear follow-up routes.
Integrating Functional Fitness into Department Culture
Leaders, make functional fitness everyday practice so you shift expectations: short mobility routines, grip and carry drills, and heart-rate bursts that mirror job demands will strengthen resilience and reduce cardiac strain across shifts.
Incorporating physical activity into weekly training drills
Schedule two short circuits into weekly drills so you build job-specific strength, interval conditioning, and recovery habits; rotate stations and track progress with simple scorecards.
Designing low-cost fitness spaces within the station
Convert an unused bay or locker area into a compact gym with mats, adjustable sandbags, bands, kettlebells, and a pull-up bar so you create accessible options that require minimal budget and maintenance.
Inside, plan zones for mobility, strength, and cardio that fit your crew’s space; you should prioritize durable flooring, visible safety signage, secure equipment storage, and a simple budget plan-shop used gear, solicit donations, and assign rotation and cleaning duties so the space stays usable and inclusive for all fitness levels.
Nutritional Leadership and Firehouse Dietary Standards
You set dietary standards that reduce cardiac risk by prioritizing whole foods, portion control, and scheduled meals; model choices during shifts and coordinate with cooks to swap fried options for grilled and plant-forward sides.
Developing guidelines for heart-healthy station meals
Create simple station meal guidelines with calorie-aware portions, reduced sodium recipes, and clear snack policies so you standardize healthier options across shifts.
Educational outreach on nutrition and long-term recovery
Offer recurring trainings that teach you how nutrition aids recovery, supports cardiac rehab, and guides medication timing; include take-home materials for firefighters and families.
Include hands-on workshops with registered dietitians, cooking demos, and printable meal plans so you translate guidelines into daily habits. Schedule one-on-one consultations after cardiac events so you tailor recovery nutrition and coordinate with medical providers. Track outcomes through periodic weight, blood pressure, and cholesterol checks so you measure program effectiveness and refine station protocols.
Addressing Behavioral Health and Stress Management
The physiological link between chronic stress and heart disease
Chronic stress accelerates heart risk by raising blood pressure, promoting inflammation, and disrupting sleep and metabolism, which increases arrhythmia and atherosclerosis risk. You should screen for persistent stressors during health checks, track blood pressure trends after major incidents, and connect members with medical evaluation when symptoms or uncontrolled hypertension appear.
Implementing peer support and decompression protocols
Create peer support routines that allow debriefs, short cooldowns, and rapid access to mental health resources after high-stress calls. You can assign trained peers to check in within 24-72 hours, log exposures, and ensure rest breaks to lower acute cardiovascular strain.
Train your selected peers in psychological first aid, active listening, and basic cardiovascular warning signs so they spot high-risk members. Develop clear post-incident steps: immediate safety and rest, a 10-30 minute team decompression, followed by scheduled follow-ups at 24 hours and one week. Integrate quick physiological checks-blood pressure, heart rate-and pathways for expedited medical referral or occupational health evaluation when readings or symptoms exceed set thresholds.
Securing Funding for Wellness Initiatives
You should prioritize diverse funding streams-grant proposals, local appropriations, and fundraising-to underwrite screenings, AEDs, and fitness programs; create clear budgets, measurable goals, and success metrics to strengthen applications and board buy-in.
Navigating AFG and state-level health grants
Apply for AFG and state health grants by aligning proposals with program priorities, documenting training needs, and submitting clear equipment justifications; include outcome measures and letters of support from local EMS or hospitals to increase competitiveness.
Leveraging community partnerships for equipment and resources
Tap local businesses, civic groups, and foundations for donated AEDs, fitness equipment, or clinic space; offer public recognition, training partnerships, and shared maintenance plans to secure long-term support.
Build formal partnerships by drafting MOUs that specify responsibilities, maintenance schedules, and liability coverage; prepare one-page proposals tailored to each partner’s interests, offer training or branding opportunities, coordinate grant-matching or tax-deduction documentation, and track donations with outcome data so you can demonstrate impact and retain support.
Summing up
With this in mind you should champion regular screening, CPR/AED training, clear protocols, and a culture that prioritizes cardiac readiness, set measurable goals, assign responsibilities, and secure partnerships to reduce on-duty cardiac events and protect your team.
FAQ
Q: How can volunteer fire chiefs assess their team’s cardiac health risks and needs?
A: Volunteer fire chiefs should begin by collecting basic demographic and medical-history information with informed consent and clear confidentiality safeguards. Crew incident logs and absenteeism patterns can reveal trends in exertional events or heat-related problems. Simple on-site screenings for blood pressure, resting heart rate, weight/BMI, and glucose can identify members who need medical follow-up. Partnering with a local occupational health provider or community clinic helps arrange deeper testing such as lipid panels and ECGs for high-risk individuals. Chiefs should use the collected data to prioritize interventions, set measurable goals, and document referrals and follow-up actions.
Q: What training, equipment, and operational policies should chiefs implement to reduce on-duty cardiac events?
A: Chiefs should ensure universal CPR and AED training with hands-on practice and quarterly refreshers for all members. Strategic AED placement, a maintenance and testing schedule, and a clear AED-use protocol must be established and logged. Implementation of heat-illness prevention measures, structured rehab and cooling procedures during prolonged incidents, and scheduled hydration and rest rotations reduce physiologic strain. A medical response protocol that defines on-scene assessment, immediate treatment steps, and transport triggers improves outcomes. Return-to-duty medical clearance policies and defined fitness-for-duty criteria protect both the individual and the organization.
Q: How can chiefs sustain a long-term cardiac health initiative, secure resources, and measure success?
A: Chiefs can pursue grant funding, municipal budget allocations, and community fundraising to cover screening, training, and AED costs. Building partnerships with local hospitals, EMS agencies, public health departments, and occupational-health clinics provides access to expertise, referral pathways, and sometimes in-kind services. Routine annual or biannual screenings coupled with wellness offerings such as exercise guidance, smoking-cessation resources, and weight-management referrals support ongoing risk reduction. Tracking metrics such as screening participation rate, number of identified high-risk members, AED deployment outcomes, on-duty cardiac incidents, and time-to-CPR/AED provides objective measures of program impact. Regular review meetings to analyze data, adjust priorities, and share success stories maintain leadership visibility and member buy-in.